What is a craniopharyngeoma?
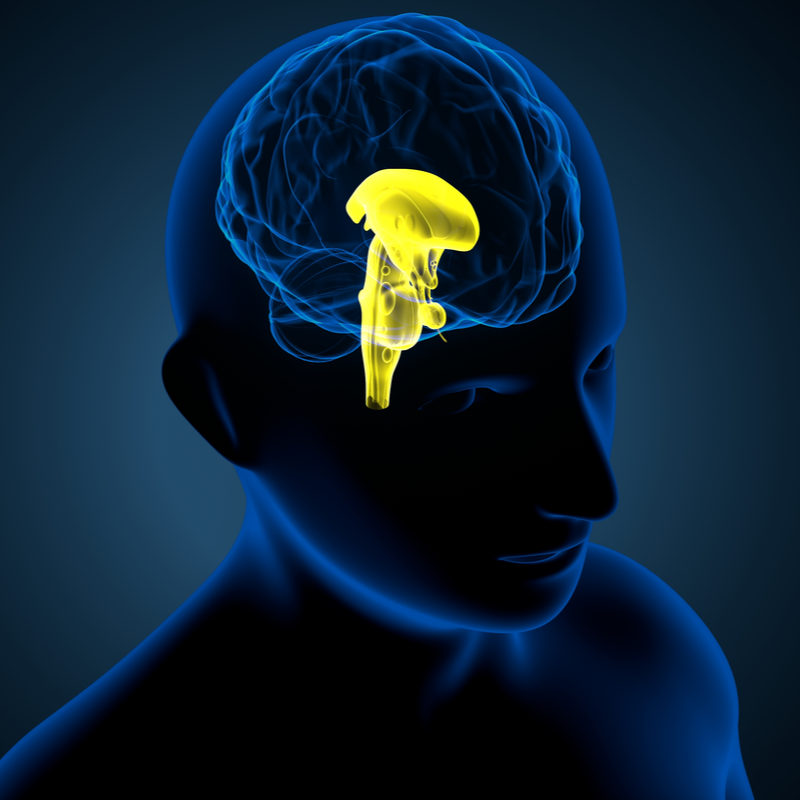
Craniopharyngeomas are tumours, that develop in the area of the stalk of the pituitary gland. These tumours are benign and also grow quite slowly, but they can become very fused with surrounding structures, such as the pituitary gland, optic nerves, pituitary stalk and blood vessels.
How common is a craniopharyngeoma?
About 2.5 to 4 % of all brain tumours are craniopharyngeomas and about half occur in childhood, usually between the ages of 5 and 10 years. The other 50% of these tumours develop in adults, especially after the age of 40.
Who is particularly affected by a craniopharyngeoma?
Craniopharyngeomas affect both men and women.
How does a craniopharyngeoma develop?
Craniopharyngeomas develop when the residual cells of the Rathke's pouch suddenly multiply . This Rathke's pouch is a structure from the embryonic development of the pituitary gland, which normally regresses again. The craniopharyngeomas occur mainly in the area of the pituitary stalk, from where they can extend in different directions, parasellar, suprasellar or sellar. Only about 5 % of all craniopharyngeomas grow only intraventricularly.
Two forms of craniopharyngeomas are distinguished by medical experts:
- Adamantinous Craniopharyngeoma, which occurs particularly in children. It is often calcified and hard and has a particularly high risk of recurrence.
- Papillary Craniopharyngeoma, which occurs mainly in adults . It is very rarely calcified and has a much lower risk of recurrence.
What are the symptoms of a craniopharyngeoma?
A craniopharyngeoma is basically a benign tumour, but depending on its size and location, it can sometimes cause dangerous symptoms. For example, if the craniopharyngeoma presses on the optic nerve, visual disturbances can be the result. In most cases, the visual fields in the outer area are lost at first. Some people even go blind if the tumour is very large.
Early signs of a craniopharyngeoma are, in most cases, difficulty concentrating, deterioration of memory and changes in personality. Mostly these symptoms appear months before the diagnosis is made. In children, such a tumour is usually noticeable by the absence of puberty or by a disturbance in growth. The reasons for this lie in a disturbance of the hormone balance.
How are craniopharyngeomas diagnosed?
The first choice as a diagnostic procedure is the MRI or the MRI with the use of contrast medium. This MRI image gives precise information on the localisation and extent of the tumour. A complementary CT can be helpful to detect the presence of calcifications. Whenever a craniopharyngeoma is suspected, endocrinological diagnostics are also carried out. This is used to diagnose any hormonal disorders so that they can be treated . If the MRI image shows that there is contact with the optic chiasm , which is the site that crosses the optic nerve, an ophthalmological examination must be done.
How is a craniopharyngeoma treated?
Due to displacing growth, these tumours can cause permanent damage to the surrounding brain structures. Therefore, surgical removal of the entire tumour is the best choice of therapy. If complete removal is not possible because of the proximity to the most important structures, accompanying radiosurgery or radiotherapy should be performed. This therapy can significantly reduce the risk of recurrence .
Researchers are currently working at full speed on the development of chemotherapeutic agents that could be used as a complementary therapy . Such drugs are currently being tested for the therapy of papillary craniopharyngeoma. These are BRAF inhibitors such as dabrafenib and vemurafenib.
Meanwhile, there are two surgical approaches to removing a craniopharyngeoma:
- the transcranial approach: this involves opening the skull , the craniotomy. The tumour can then be removed microsurgically . For purely intraventricular craniopharyngeomas, the is the recommended technique.
- the transnasal, transsphenoidal approach: Here, the surgical access route is via the nose. The craniopharyngeoma is also removed microsurgically here .
What are the risks of resecting a craniopharyngeoma?
Possible complications after resection can include, in particular, disturbances of the hormone and electrolyte balance. However, these disturbances are usually only of a temporary nature. In a few cases, the disturbances are also permanent. After the operation, the water balance and also the blood values are checked at close intervals.
What is the prognosis of a craniopharyngeoma?
The chance of curing a craniopharyngeoma is very good and the life expectancy is significantly improved if the tumour can be completely removed at an operation. Equally important for the prognosis is that hormone replacement therapy is successful. If the hypothalamus is also affected, the prognosis is much worse.
What is the life expectancy for a craniopharyngeoma?
The depending on how early the tumour was discovered, the better or worse the prognosis. It also depends on whether the tumour could be completely removed during an operation. If the craniopharyngeomas are still compact, small and operable, the prognosis is good in the long term. However, 80 to 90 % of those affected suffer permanent hormone deficits. This is why these people then have to take preparations as hormone replacement for the rest of their lives. Under certain circumstances, these preparations trigger secondary diseases that can have an enormous impact on the quality of life . Around 30 % of people with a craniopharyngeoma are obese. Therefore, the risk for diseases such as diabetes mellitus and cardiovascular diseases is particularly high.
If a craniopharyngeoma is surgically removed and followed by radiation, the cure rate after 10 years is 70 to 83 %. Despite this, hormone deficits are one of the most frequent possible consequences of radiation. The prognosis is much worse if the hypothalamus is affected. In this case, an adapted diet and regular physical exercise are indispensable to reduce mortality due to the consequences of the therapy. If disturbances of vision, memory and concentration have already developed before the operation, these cannot be remedied in most cases by an operation.
