Causes of tumours
Tumours, so-called neoplasms of body tissue, can be benign or malignant. In layman's terms, malignant tumours are called cancer, although this term includes many different diseases. All cancers have in common that the body cells change (degeneration) and grow uncontrollably. This destroys the tissue in the vicinity of the tumour. But it is also possible for cancer to spread throughout the entire body through the so-called formation of metastases. But how can tumours form in the first place?
How do cancer cells develop?
Until now, doctors have not been able to clearly explain how healthy body cells become cancer cells. However, they are certain that altered genetic material in a previously healthy cell or errors in cell division play a significant role in the formation of tumour cells. In order to understand the latter, one has to understand how cell division takes place. The cell contains the genetic material, i.e. all important information about function and appearance. During cell division, the genetic information contained in the cell doubles and is distributed to two daughter cells. If errors occur during this division, a damaged daughter cell emerges. This damaged daughter cell (potential cancer cell) is controlled by the body's own immune system and destroyed if necessary in order to prevent further cell division. If this self-destruction does not take place, for example in patients with a weakened immune system, the potential cancer cell can continue to divide and multiply. Over time, a tumour develops that is either benign or malignant.
How do healthy cells differ from cancer cells?
Unlike healthy body cells, cancer cells do not perform any function in the organism. Instead, they differ from normal cells in terms of how they divide and grow, behave differently from healthy cells when they age and die, and can settle in other tissue cells and continue to grow there (metastasis).
What role do oncogenes and repair genes play in the development of cancer?
Oncogenes, tumour suppressor genes and repair genes also occur in healthy body cells and determine the growth and maturation of the cells. While oncogenes promote cell growth, tumour suppressor genes suppress growth. If changes, so-called mutations, occur within the oncogenes or the tumour suppressor genes, the repair genes can normally repair the damage. However, if the damage cannot be regulated, cell division occurs even when the body does not need new cells. This sets in motion an uncontrolled growth of cells, which in turn leads to an excess of tissue and can manifest itself externally in a growth (tumour).
Which factors favour cancer cells in their development?
It has already been possible to determine some risk factors that favour pathological changes during cell division. These include, among others:
- an unhealthy lifestyle, i.e. unhealthy diet, lack of exercise and/or excessive alcohol and tobacco consumption,
- harmful environmental influences such as inadequate air and water conditions,
- Infections with viruses: these include mainly the human papillomaviruses (HPV) as well as herpes and adenoviruses,
- Contact with chemicals or other carcinogenic substances
In addition to these risk factors, the human organism is exposed to a variety of substances in the course of life that can damage the genetic material. This is why the probability of developing cancer increases with age.
Tumour markers to detect cancer
Tumour markers are substances in the blood that are found in higher concentrations in the blood when cancer is present. This is because the tumour markers are produced either by the cancer cells or by the body in response to the tumour. On the basis of the corresponding tumour markers, the attending physician can determine how far the cancer has already progressed and order a suitable therapy. The tumour markers can also be used in the event of a relapse (recurrence).
Tumour markers include certain proteins, hormones or antigens that also occur in healthy people within certain limits and can be influenced by inflammation, for example. The most important tumour markers include:
- AFP (alpha-fetoprotein): a protein that is produced by the fetus during pregnancy, but can also show elevated levels in germ cell tumours of the ovaries and testis, liver tumours and hepatoblastoma
- CA 15-3: is mainly produced in breast cancer, cirrhosis of the liver and/or inflammation of the body
- CA 19-9: can only be measured in people with certain blood groups and occurs in tumours of the pancreas, liver, bile ducts, stomach, colon and rectum
- CA 72-4: occurs in stomach cancer, certain forms of ovarian cancer and pancreatic cancer
- CA125: indicates a tumour of the ovaries, but can also increase during pregnancy
- Calcitonin: is produced in the thyroid gland and can indicate certain thyroid tumours
- CEA: is produced by cancer of the colon or rectum, a stomach tumour, a tumour in the female breast or in the lungs
- hCG (human chorionic gonadotropin): can be produced by tumours of the testis or ovaries
- NSE (neuron-specific enolase): is an enzyme that is produced during sugar metabolism and can indicate certain forms of lung cancer (bronchial carcinoma)
- PSA (prostate-specific antigen): is formed by the prostate as a sugar-protein and can indicate prostate cancer if the values are elevated
- TG (thyroglobulin): is a thyroid hormone and can indicate thyroid cancer
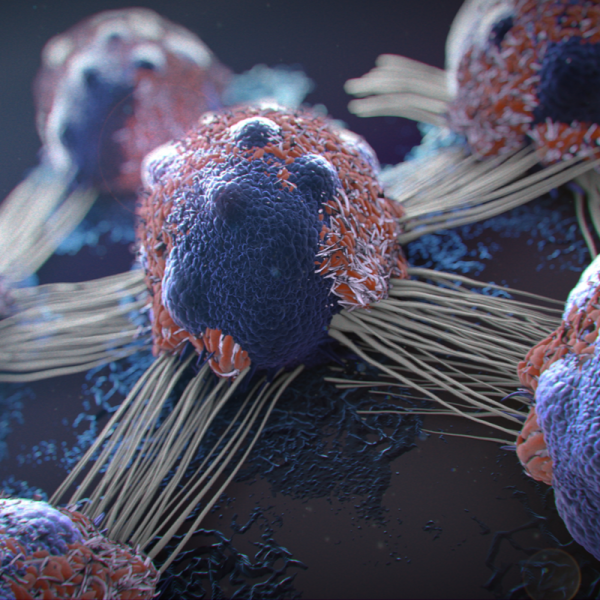
How does the immune system react to tumour cells?
Because tumour cells are fundamentally different from healthy cells, the immune system is also able to recognise tumour cells and destroy them in time. In healthy people with an intact immune system, this also happens without the person concerned noticing anything. However, cancer cells can also develop evasion strategies to develop an appropriate immune response and thus trick the immune system. This can happen, for example, by the tumour cells making themselves invisible to the immune system or by inhibiting the immune response.
