What is a chorioangioma?
Chorangiomas are benign tumours of the chorionic tissue that makes up the embryonic covering (placenta). The extremely rare disease, which occurs in about 05, to 1 percent of all pregnancies, is caused by a fetal or maternal malformation. A chorioangioma is usually detected in the second trimester of pregnancy by ultrasound (sonography) . While large chorionangiomas cause pregnancy complications, smaller chorionangiomas behave asymptomatically. In the vast majority of all cases, the latter case applies, i.e. the chorioangiomas are not clinically significant and do not affect placental function .
Chorioangiomas are the most common tumours of the placenta. Chorioangiomas with a diameter of more than 5 cm tend to occur less frequently than smaller chorionangiomas. However, it can happen that particularly small chorioangiomas cannot be made visible by ultrasound and therefore cannot be diagnosed.
How does a chorioangioma develop?
A chorioangioma develops from the primitive chorionic mesenchyme, also called chorionic mesoderm. This is a loose layer of connective tissue that is separated from the amniotic mesenchyme by a narrow, fluid-filled cleft. The formation of a chorioangioma occurs when the stroma and blood vessels begin to proliferate independently of the surrounding tissue. Chorioangiomas are vascular tumours. This means that they consist of blood vessels, although in most cases the tumour is benign.
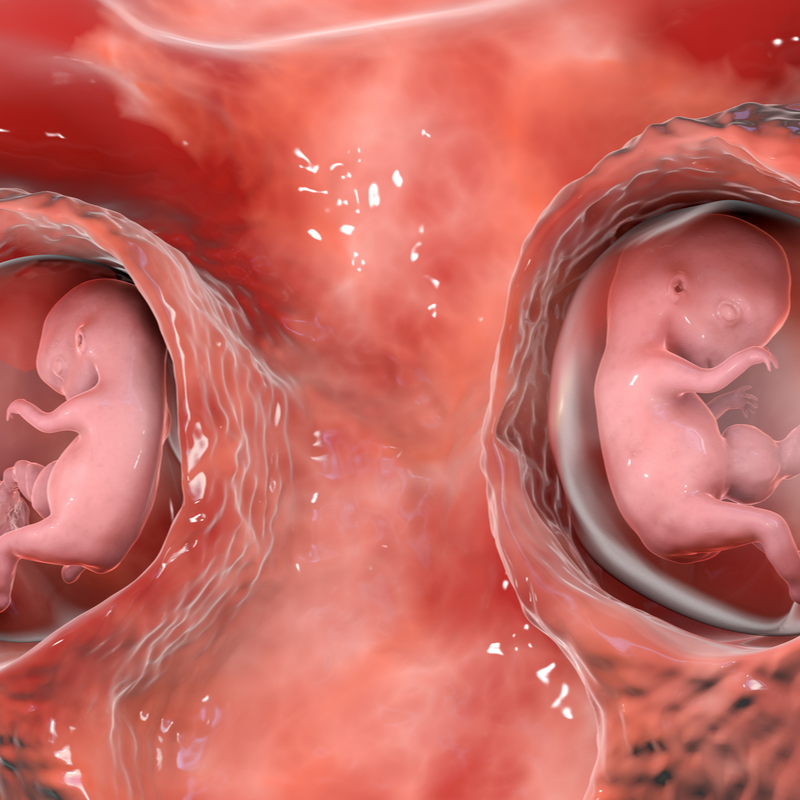
The exact cause of a chorionangioma is still unknown. However, a chorioangioma is more common in multiple pregnancies.
What are the different forms of chorionangioma?
The chorionangioma is divided into the following three types, whereby assumes that each type represents a phase of tumour development :
- cellular type: this is an immature type consisting mainly of cellular, compactly formed elements.
- angiomatous (vascular) type: occurs as the most common form of chorionic carcinoma and is typical for its numerous, small blood vessels.
- degenerative type: this is a mature type with degenerative changes.
In most cases, a chorionic angioma has no malignant potential.
What pregnancy complications can a chorioangioma cause?
If it is a chorioangioma that is larger than 4 or 5 cm, or multiple chorioangiomas, the following complications can occur during pregnancy:
- Complications for the foetus:
- Destruction or premature breakdown of red blood cells (haemolytic anaemia),
- fetal thrombocytopenia, i.e. the inability of blood to clot due to a lack of platelets,
- Blood clots in the umbilical cord (umbilical vein thrombosis),
- Occurrence of fluid accumulation and swelling in several parts of the baby's body (non-immune hydrops),
- fetal cardiomegaly: enlargement of the heart in the foetus,
- fetal heart failure, which can lead to the death of the newborn,
- fetal stroke,
- intrauterine growth retardation, which may be caused by a mass protruding into the amniotic cavity
- congenital anomalies.
- Complications for the mother:
- Occurrence of excessive amniotic fluid in the womb (polyhydramnios),
- Triggering of premature labour,
- High blood pressure together with increased protein secretion, which is also accompanied by signs of organ damage (pre-eclampsia),
- Detachment of the placenta with associated blood loss,
- Birth deformity (abnormal positioning of the baby at birth),
- necessary caesarean section,
- Fluid accumulation and swelling reflecting the health of the foetus (maternal mirror syndrome),
- postpartum haemorrhage.
Typically
small chorionangiomas behave asymptomatically and do not cause
any complications. Only after a certain size can the
chorionangioma pose a risk to the pregnancy and
the foetus in some cases.
How is a chorioangioma diagnosed?
In most cases, a chorionangioma does not cause any symptoms. As a rule, the disease is diagnosed in the second trimester scan . Here the chorionangioma is shown on the image as an echo-poor or echo rich space, which can usually be clearly distinguished from the placenta by a greyscale ultrasound scan . However, some chorionic angiomas, which appear as a solid mass, may not be identified by a greyscale ultrasound scan and remain undetected, especially if they are also asymptomatic. It can even happen that a small chorionic angioma is only discovered after birth, when the placenta is examined.
If, on the other hand, it is a larger chorionangioma, fibrous septa (dent-like appearance) can also be seen. A chorionangioma protrudes into the amniotic cavity (part of the embryonic blastocyst) near the formation of the umbilical cord.
How is a chorionangioma treated?
A chorionangioma is initially only observed, as they usually behave asymptomatically anyway. If it is a large chorioangioma, it is checked by ultrasound at intervals of one to two weeks in order to monitor the tumour growth, but also the amniotic fluid level as well as the fetal heart function and the growth of the foetus. Should complications arise, the following treatments may be used:
- Administration of fetal transfusions,
- fetoscopic Laser coagulation of tumour-supplying vessels: Under local anaesthesia, a 1.9 millimetre thin light source (fetoscope) is brought into the amniotic cavity through the mother's abdominal wall in order to specifically obliterate the tumour vessels.
- endoscopic surgical devascularisation,
- Chemosclerosis
What is the prognosis for a choriangioma?
In large choriangiomas, which have both reduced echogenicity and reduced tumour volume as well as reduced blood flow in the colour double image, they may suffer a spontaneous infarction. In chorioangiomas with decreased blood flow, doctors have shown that both fetal haemodynamics are improved.
