What is Coxsackie B2?
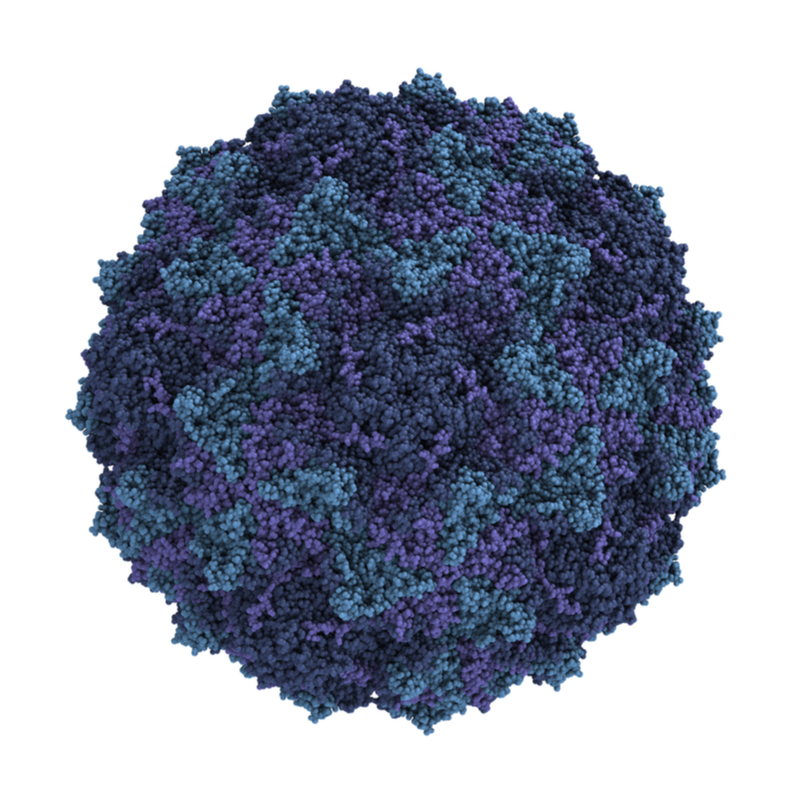
Coxsackie B2 viruses are non-enveloped single-stranded RNA viruses. They belong to the family of picornaviruses. They are the main cause of diseases such as colds, myocarditis and meningocarditis. The viruses have a size of about 20 - 40 millimetres and possess only a single RNA strand. Coxsackie B2 viruses have no envelope, their genome is enveloped in a cubic capsid. They have a high stability and survival rate in acidic environments and are only sensitive to chlorine-containing disinfectants. Instead, alcohol-based disinfectants have no effect on coxsackie viruses. At room temperature they can survive for several days and can also be contagious.
How is the Coxsackie B2 virus transmitted?
The transmission of Coxsackie B2 viruses is from person to person via the faecal-oral route of infection. Sometimes they can also be passed on via droplet infections or smear infections. After the viruses have been ingested orally, they first begin to multiply in the mucous membrane of the pharynx and then in the intestinal wall. The Coxsackie B2 viruses are mainly excreted in the stool.
What are the symptoms of the Coxsackie B2 virus?
As a rule, infections with the Coxsackie B2 virus are completely symptom-free or have only very minor symptoms. The following symptoms are observed most frequently :
- Fever, similar to flu,
- Rhinitis,
- Pharyngitis,
- Nausea and vomiting.
As
accompanying symptom, gastrointestinal complaints
may also occur. Normally, the symptoms disappear after 3-4 days, in
some cases only after a week. The diseases caused
by the Coxsackie B2 virus occur most frequently in summer
and early autumn.
Coxsackie B2 viruses are the main cause of the following diseases:
- aseptic meningitis,
- Encephalitis,
- Paralysis,
- Exanthema
- Generalised disease in the newborn,
- Hand-foot-and-mouth disease,
- Herpangina,
- Pericarditis, myocarditis,
- Pneumonia,
- Pleurodynia.
Meningitis and encephalitis
Especially in children, Coxsackie B2 viruses are the cause of aseptic meningitis. The viruses occur particularly frequently in summer and autumn, in regions with a mild climate. Affected persons develop acute symptoms such as chills, headache, high fever, photophobia, nausea and vomiting, and pain when moving the eyes. Other symptoms may include cough, pharyngitis, diarrhoea, myalgias, pleurodynia, herpangina and myocarditis.
In rarer cases, encephalitis occurs. Symptoms include seizures, disorientation and increasing lethargy. People with an intact and strong immune system have an excellent prognosis. Patients, who have agammaglobulinemia, hypogammaglobulinemia or other severe immunodeficiencies, are at risk of chronic encephalitis or meningitis. About 50 % of those affected suffer from symptoms similar to those of dermatomyositis, such as exanthema, oedema and myositis. Chronic hepatitis may also develop.
How are Coxsackie B1 viruses diagnosed?
Depending on the clinical picture, a diagnostic measure is selected. If it is an acute phase of the infection, molecular biological evidence in stool, pharyngeal lavage and cerebrospinal fluid can be provided with the help of a PCR test. Serological examinations alone can indicate an increase in the corresponding titre, however, this examination is not sufficient for making a diagnosis.
How is Coxsackie B2 virus treated?
Mostly the treatment of diseases caused by Coxsackie B2 viruses is symptomatic with antipyretics and analgesics. If a severe course manifests itself during the disease, gamma-globulin preparations can be used. If a secondary bacterial infection occurs, the choice is antibiotics. Currently, the antiviral drugs are still being tested, but the drug interferon, which is used in cardiomyopathy, has been shown to be very effective and efficient .
Especially in the first weeks after infection, patients are highly infectious, i.e. highly contagious. The Coxsackie B2 viruses can still be excreted in the stool for several weeks, even if the symptoms have long since disappeared. This is why people with an infection are considered to be contagious for a very long time. In order to avoid transmission of the Coxsackie B2 virus, it is essential that the hygiene regulations are meticulously observed even after the symptoms have subsided.
What is the prognosis for the Coxsackie B2 virus?
The course of the disease is usually mild, which is why only symptomatic treatment is usually administered. Normally, those affected can recover excellently from the disease, but it is still possible for complications to develop, such as pericarditis, myocarditis or meningoencephalitis.
How can Coxsackie B2 viruses be prevented?
To prevent Coxsackie B2 virus infection, it is important to take the following measures:
- Especially in the neonatal unit of a hospital, the efficient hospital hygiene should be applied, which means: a suitable antiviral disinfectant, regular gown changes and nappy hygiene. It may be necessary to isolate infected newborns.
- Post-exposure prophylaxis, which means that gamma globulin must be administered within 72 hours, if there is a particularly high risk.
- Exposure prophylaxis, which means using proper hand hygiene. First wash hands thoroughly with warm water and soap and then disinfect.
Is there an obligation to report the Coxsackie B2 virus?
As of today, there is no obligation to report the virus. However, if outbreaks accumulate , a report must be made to the public health department by the respective laboratory manager. Once the disease has been overcome , the patient has lifelong immunity. There is currently no vaccination against the Coxsackie B2 virus.
