What is Coxsackie B6?
The Coxsackie B6 viruses belong to the picornavirus family like the hepatitis A virus . They are single-stranded RNA viruses and belong to the enterovirus genus. They can be found all over the world, but are more prevalent where the climate is mild, such as in Central Europe. The peak of the disease is in the late summer and early autumn. During these periods, epidemic outbreaks can occur . After infection with the virus , IgM antibodies can be detected in the blood after about 7 to 10 days and can remain there for a month. A second serum sample is indispensable in order to be able to observe the rise in the titer .
How is Coxsackie B6 transmitted?
Coxsackie B6 viruses are mostly transmitted from person to person via the faecal-oral route . However, transmission through smear infections and droplet infections are also possible. If a person has been infected orally, i.e. has ingested the viruses, they will first multiply in the pharyngeal mucosa and then in the intestinal wall before being excreted from the body via the stool.
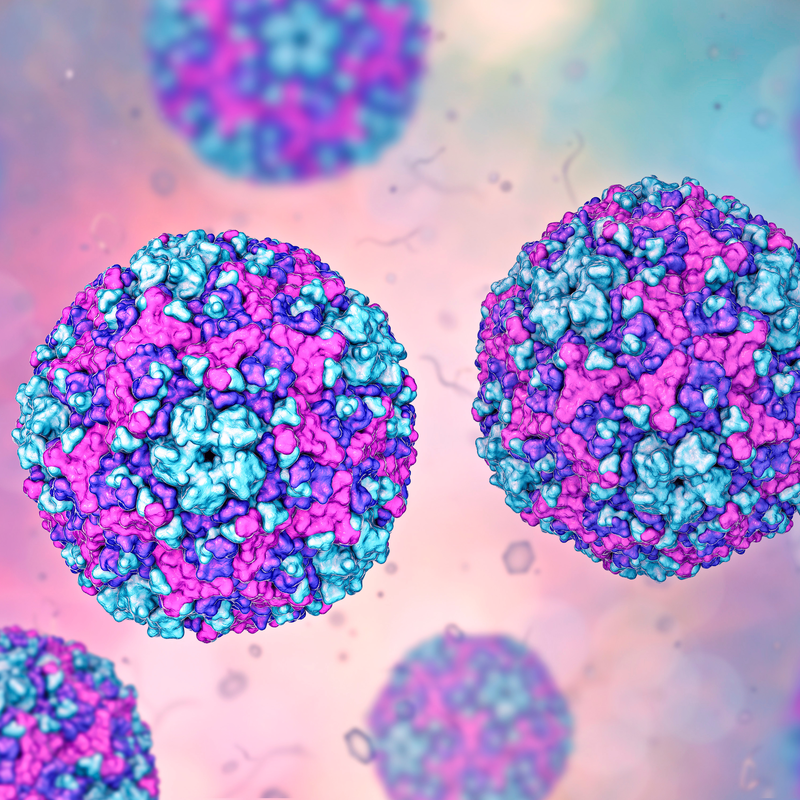
What is the morphology of Coxsackie B6 viruses?
The viruses are about 20-40 mm in size and have a positive polarising single-stranded RNA. A viral envelope is not found in the Coxsackie B6 viruses. Their genome is enveloped in a cubic capsid . They exhibit an enormously high stability and survival rate in particularly acidic environment. They are only sensitive to chlorine-containing disinfectants. This means that conventional disinfectants based on alcohol or detergents are completely ineffective. They are not eliminated at all and can survive for days at room temperature and be infectious.
What are the symptoms of Coxsackie B6 virus?
A Coxsackie B6 infection usually runs its course without symptoms or only with minor symptoms. After an incubation period of about six days , fever, general malaise and headache occur. In many cases, there are accompanying symptoms such as pharyngitis, rhinitis, vomiting and nausea, and symptoms of mild gastroenteritis are also not uncommon. Usually, the symptoms disappear after about four days, but they rarely last longer than a week.
Pleurodynia
It is also called Bornholm disease or epidemic myalgia. The disease becomes noticeable through acute rising fever, cramp-like and stabbing chest pain . Children in particular may also experience pain in the upper abdomen. The attacks usually last 15-30 minutes and are often accompanied by tachypnoea and sweating . Fever peaks about an hour after the attack begins , but quickly decreases as the symptoms subside . Affected people complain of painful muscles. A pleural rub is often heard on auscultation. However, blood count and chest X-ray are unremarkable. Most cases of pleurodynia are caused by Coxsackie B6 viruses. As a rule, the symptoms improve within a few days and a recurrence is rather rare. Treatment involves the administration of NSAIDs , i.e. non-steroidal anti-inflammatory drugs. Other measures such as heat treatment of the affected regions can be carried out to accompany the therapy.
How are Coxsackie B6 viruses diagnosed?
The diagnostic measures depend on the clinical picture. In an acute phase, it is possible to obtain evidence in the stool, pharyngeal lavage fluid and in the cerebrospinal fluid by means of a PCR test. A serological examination is not sufficient to make a diagnosis. However, a rise in the titre can be wonderfully indicated with the help of serological tests.
How is Coxsackie B6 virus treated?
The therapy of the disease caused by Coxsackie B6 virus, is in most cases treated symptomatically. This means that antipyretics and analgesics are taken when needed. If the course of the disease worsens, gamma globulin preparations can be used. If a secondary bacterial infection is detected, antibiotics are used. Currently, drugs with antiviral effects are still being tested. The drug interferon, which is used especially in cardiomyopathies, has proven to be very suitable .
How long is the Coxsackie B6 virus contagious?
Particularly in the first weeks of the disease, an affected person is highly infectious. But even after the symptoms and complaints have subsided, the virus continues to be excreted in the stool for weeks. In view of this, a patient is still contagious for a very long time and the hygiene regulations must still be observed even when the symptoms have completely disappeared. This is the only way to prevent the virus from spreading .
What is the prognosis for the Coxsackie B6 virus?
The course of the disease is mild in most cases and can only be treated symptomatically . As a rule, patients recover well from the infection. However, complications such as meningoencephalitis, meningitis, myocarditis or pericarditis should always be expected.
How can the Coxsackie B6 virus be prevented?
The following measures are important and can help prevent Coxsackie B6 virus infection:
- An efficient hospital hygiene, especially on the neonatal ward, i.e.: antiviral effective disinfectants and not those based on alcohol or detergents, sufficient nappy hygiene and gown changes. If necessary, infected newborns must be isolated.
- Exposure prophylaxis, which means practising adequate hand hygiene. First wash hands thoroughly and then disinfect.
- Post-exposure prophylaxis, which means giving gamma globulins within 72 hours if there is a particularly high risk.
Individual
detections of the Coxsackie B6 virus do not have to be reported according to
Infection Protection Act. However, if the
infections accumulate, the responsible laboratory director must issue a report to the
health department. A patient who has had the infection once
is considered immune to the Coxsackie B6 virus. There is currently no
vaccination.
