What are endometrial polyps?
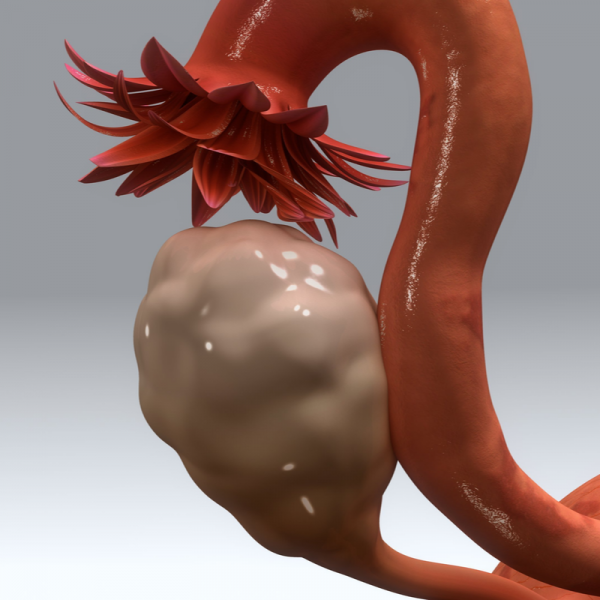
Endometrial polyps develop within the mucous membrane that lines the inside of the uterus, called the endometrium. Endometrial polyps are cellular formations consisting of the glands of the endometrium, blood vessels and stroma that emerge from the endometrial cavity. About 20 per cent of all women, especially between the ages of 40 and 65, develop endometrial polyps, which can spread through the uterine wall.
What types of endometrial polyps are there?
Endometrial polyps are differentiated according to their number, size, location within the uterus and histological structure. As a rule, endometrial polyps are benign; only between 0.5 and 1 per cent of all endometrial polyps can degenerate into cancer. However, predisposing factors such as obesity, the onset of menopause, hormone therapy with oestrogen etc. also play a role here.
What causes play a role in the development of endometrial polyps?
The following risk factors can favour the development of endometrial polyps:
- an increased oestrogen level, but also a hormonal imbalance,
- hormone therapy with oestrogen without a corresponding hormone balance with progesterone,
- taking the drug tamoxifen,
- increasing age,
- Obesity..,
- High blood pressure,
- past colon cancer
In order to diagnose endometrial polyps in time, patients should have an annual gynaecological examination.
What are the symptoms of endometrial polyps?
Endometrial polyps are usually asymptomatic, but in some cases they can cause irregular uterine bleeding. These can manifest themselves, for example, as heavier menstruation, postmenopausal bleeding or bleeding after sexual intercourse. If the polyps are particularly large, they can also cause pain in the lower abdomen, which can be accompanied by small contractions of the uterus. In rare cases, polyps larger than one centimetre in diameter can cause infertility or miscarriage.
How are endometrial polyps diagnosed?
Endometrial polyps are usually diagnosed by chance during a transvaginal ultrasound examination. If endometrial polyps are suspected, the gynaecologist can also perform a 3D ultrasound examination or a hysterosonography. The latter examination method involves the administration of saline solution into the endometrial cavity to make the polyps visible on ultrasound.
How are endometrial polyps treated?
Endometrial polyps that are larger than 1 cm are usually removed surgically. This procedure is also recommended for patients who suffer from infertility or have already suffered a miscarriage. Smaller endometrial polyps can be removed by hysteroscopy, although it is not always necessary to put the patient under general anaesthetic
.
| Pathogen | Source | Members - Area |
|---|---|---|
| Endometrial polyps | EDTFL | As a NLS member you have direct access to these frequency lists |
