What is fibrosis?
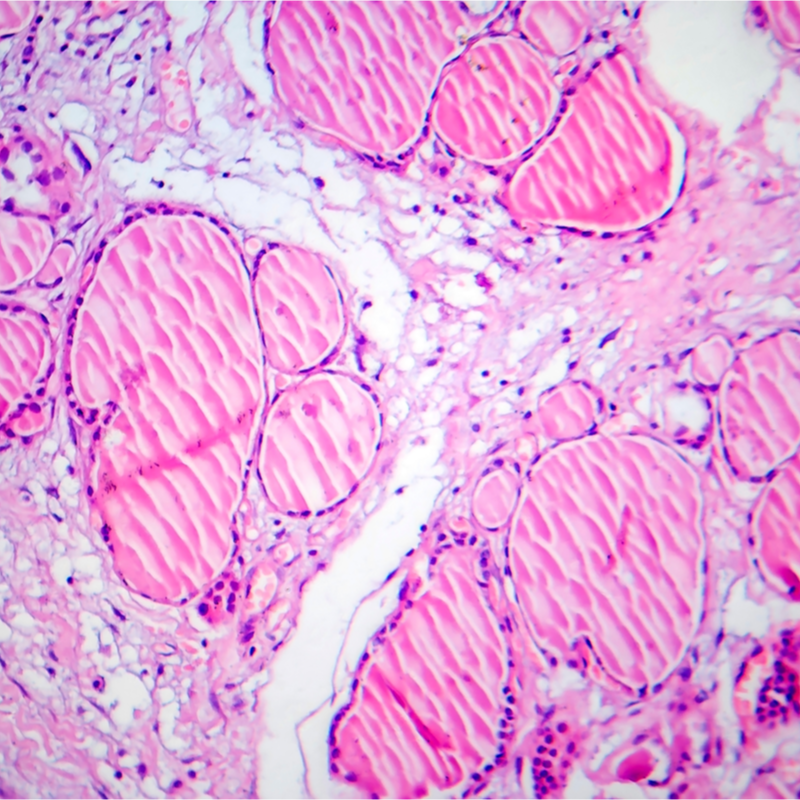
Fibrosis or sclerosis is a tissue change and is characterised by the proliferation of connective tissue cells and collagen fibres. As a result, the connective tissue appears hard and less elastic and only fulfils its tasks to a limited extent. The disease can manifest itself in individual tissues, but also organs, and even entire organ systems.
What forms of fibrosis are distinguished?
Doctors commonly distinguish between the two forms of fibrosis:
- primary Fibrosis: This is a rather rare, spontaneously occurring fibrous proliferation, i.e. a disease that occurs without any recognisable cause.
- secondary fibrosis: This form of fibrosis is more common and describes a fibre proliferation that is triggered by endogenous or exogenous triggers, such as inflammation, infection or ischaemia (reduced blood flow to tissue).
Fibrosis,
which manifests itself in organs, can be associated with an increasing
loss of function of the tissue. The following diseases of the
organs can manifest themselves through the development of fibrosis
:
- endomyocardial fibrosis: describes a thickening of the muscular wall of the heart (myocardium), which can contribute to a stiffening of the heart muscle. Endomyocardial fibrosis mainly affects the ventricle (diastole).
- Haemochromatosis: This is an iron storage disease that causes the body to become overloaded with iron. The deposition of excess iron in organs and tissues can lead to damage.
- Hedinger syndrome: occurs through the so-called carcinoid syndrome and affects and can lead to tricuspid regurgitation of the right ventricle.
- H63D syndrome: is based on the mutation of the HFE gene and can cause various clinical pictures.
- Capsular fibrosis: can occur as a result of the insertion of a breast implant and describes the development of a hard connective tissue-like capsule, which is sometimes painful.
- Liver fibrosis: contributes to the development of cirrhosis, where the tissue becomes knotty and hard and contracts tightly , reducing the size of the liver. Active liver cells are displaced, which causes the organ to lose function and can manifest itself , for example, through fluid retention in the abdomen. In the worst case, the liver loses its complete function, leading to the so-called fatal coma hepaticum.
- Pulmonary fibrosis: are in most cases due to chronic inflammation and can become noticeable through shortness of breath and/or a dry cough . In the worst case, pulmonary fibrosis leads to complete loss of function of the lungs.
- Mediastinal fibrosis: usually asymptomatic disease in which there may be a granulomatous inflammatory process in the mediastinum.
- Osteomyelofibrosis: describes a pathological change in the bone marrow tissue, resulting in disturbances in blood formation.
- retroperitoneal fibrosis: is a chronic inflammatory disease of the posterior abdominal cavity, which occurs rather rarely.
- Skeleroderma: is a hardening of the skin caused by a chronic inflammatory process in the vascular and connective tissue system . Skeleroderma manifests itself through restricted movement of the fingers, which can be explained by the increasing thickening of the skin. Swallowing difficulties can also be the result due to a loss of elasticity of the oesophagus. If skeleroderma also affects the internal organs, it can lead to kidney or lung insufficiency.
Due to the
proliferation of connective tissue cells (fibroblasts) and the storage
of collagen, the organ may completely lose its function,
which, in the worst case, may even result in the patient's death.
How does fibrosis develop?
A fibrosis develops following approximately the same physiological processes of scarring. Here, due to tissue damage, macrophages (white blood cells) are released, which secrete growth factors and various cytokines (proteins that play an important role in the immune defence ). These in turn activate cellular signalling. These in turn activate cellular signalling pathways, which lead to an increase in fibroblasts, or myofibroblasts . Their task is to produce collagen and glycosaminoglycans, which in this way compact the extracellular matrix of the affected tissue. While the scar formation process is completed at some point, there is no termination in the formation of fibrosis . This in turn has the consequence that more and more tissue is displaced or replaced by the fibre proliferation.
How does fibrosis develop?
Fibrosis is often caused by chronic inflammation or excessive wound healing. In addition, a variety of autoimmune diseases such as lupus erythematosus, but also vascular inflammation and/or rheumatic diseases can attack the internal organs and contribute to the development of fibrosis there.
What are the symptoms of fibrosis?
The symptoms of fibrosis depend on the type of fibrosis.
How is fibrosis treated?
There are no treatments yet that can stop the targeted proliferation of connective tissue. However, the following medicines can be given to inhibit chronic inflammation and delay the development of fibrosis:
- Glucocorticoids,
- Immunosuppressants,
- non-steroidal anti-inflammatory drugs
In addition
acetylsalicylic acid, calcium antagonists and prostacyclins can improve the
microcirculation. However, all drug therapies must be
administered for a longer period of time and can also have
undesirable side effects. In general, the
type of treatment for fibrosis always depends on the underlying disease
.
What is the prognosis for fibrosis?
Since fibrosis cannot be completely cured, it is even more important that the disease is treated as early as possible in order to minimise the damage caused by the disease. If fibrosis is only diagnosed in the final stage, organ transplantation may still be an option. If fibrosis is left untreated, the disease is always fatal. With the right treatment, the course of the disease can be delayed. In general, the prognosis of fibrosis always depends on various factors, but the disease usually has a rare favourable outlook.
