What is granolumatoid inflammation?
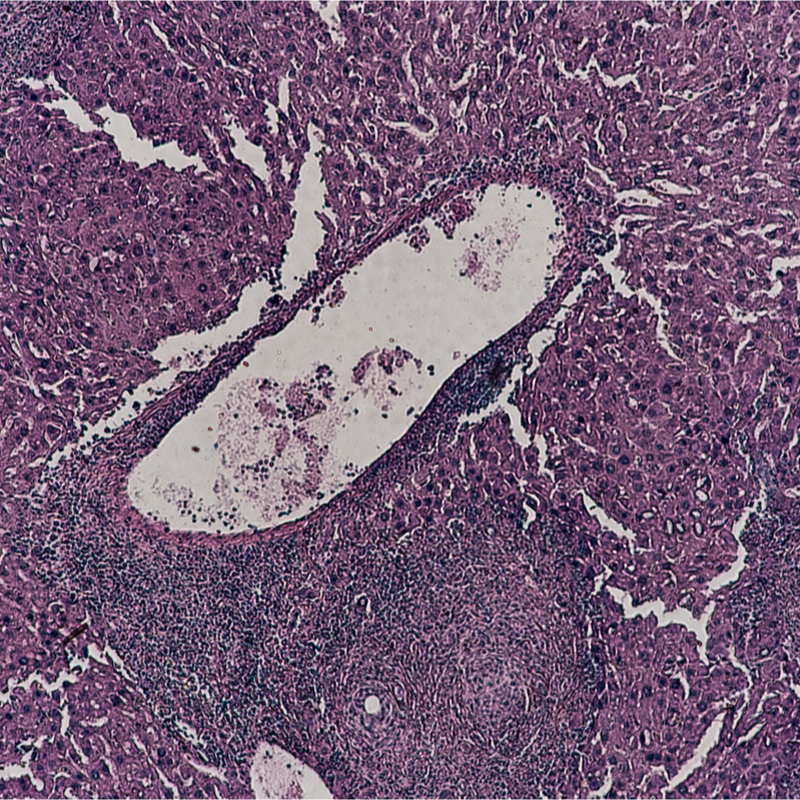
This is a form of chronic inflammation, whereby it is characterised by the appearance of small granulomas, collections of cells. Granulomatous inflammation can have a non-infectious or an infectious cause . If a pathogen cannot be destroyed by the immune system at all or only quite poorly, granulomatous inflammation often occurs in infections. In the initial course, it usually starts as a non-specific inflammatory reaction, whereby fibrosis usually forms in the affected tissue in the further course. In this inflamed area of the tissue, cell accumulations are seen, which are called granulomas. These consist of macrophages, monocytes and lymphocytes. The granulomas can have a central necrosis for example in tuberculosis or no central necrosis, as in sarcoidosis.
Where does granulomatous inflammation occur?
Granulomatous inflammation can occur in a variety of diseases:
- Infectious diseases such as syphilis, tuberculsoe, leishmaniasis, schistosomiasis,
- Sarcoidosis,
- Crohn's disease,
- Granuloma anulare,
- Granulomatosis with polyangiitis,
- Granulomatous hepatitis.
What causes granulomatous inflammation?
Until now it has been assumed that multinucleated macrophages develop due to fusions of several cells. However, research has shown that these so-called giant cells arise from the defective division of the cells. In this case, the genetic material and the size of the cell are doubled, but the cell does not divide afterwards. The body responds to the genetic damage with these giant cells.
What are the symptoms of granulomatous inflammation?
The most common granulomatous inflammation in Germany is sarcoidosis, which is accompanied by the following symptoms:
- Fever,
- Fatigue and exhaustion,
- Weight loss,
- Pain in the limbs,
- Night sweats,
How is granulomatous inflammation diagnosed?
If a granulomatous inflammation is suspected, the very first thing the doctor will do is to take the medical history to find out the complaints etc. The next pioneering step is a PET or MRI examination. The next step is a PET or MRI examination. If the lungs are affected, this can be proven beyond doubt by means of these examinations. An infestation of the lung parachyma and the lymph nodes can be detected with the help of a high-resolution computed tomography. Especially in the case of sarcoidosis, these imaging methods are indispensable, because usually the exact extent of the infestation cannot be detected and proven by checking the lung function, especially if only a fine nodular shadowing pattern is present. With the help of an MRI, an involvement of the central nervous system and the heart can be detected and also checked in the further course. The whole-body MRI can be used to look for organ involvement . This can show all active and inflammatory involvement in the organs.
Furthermore, a laboratory examination is used. The following values are determined in the laboratory:
- Measurement of calcium concentrates in the blood and urine,
- Urea and creatinine in the serum,
- GOT, CPT, gamma-GT, AP.
How is granulomatous inflammation treated?
Granulomas form mainly due to persistent irritants, whether infectious or non-infectious in origin. The body cannot turn off these inflammatory stimuli , so the current treatment strategy for non-infectious granulomas is to slow down the patient's immune system . However, this increases the risk of infections. However, this increases the risk of infections enormously. Based on the above-mentioned research, scientists now hope to be able to initiate new therapy methods that, on the one hand, prevent granuloma formation and, on the other hand, significantly improve the therapy methods for granulomatous inflammations. As the administration of corticosteroids has serious side effects, it is initially only used for the next 6 months. In the course of another 6 months the dose is then gradually phased out again. A immunosuppressive combination therapy with methotrexate and azathioprine can be considered. These are usually used in therapy to save corticosteroids. However, in younger people who still want to have children, this use is very problematic. This is because the risk of bone marrow and liver damage is significantly increased, especially with long-term administration of the drugs. Gastrointestinal side effects can also occur with both drugs. These are usually fulminant and occur quickly after the start of therapy .
What is the prognosis for granulomatous inflammation?
The prognosis is quite good in most cases. Even a spontaneous healing, especially in the case of asymptomatic organ infestation and the Löfgen syndrome, is very high at 85 %. Most of the spontaneous cures occur in the first six months after the onset of the disease. After the first year of diagnosis, a follow-up should be carried out at intervals of 3 months. Should the course prove to be good without an indication for therapy, it is important to carry out a check-up annually in the further 3-5 years. Despite immunosuppressive therapy, about 10 % of those affected develop a progressive course of the disease. The long-term administration of corticosteroids is a considerable problem. Often, enormous obesity develops from this and, as a consequence, the further complications of the metabolic syndrome.
The mortality rate is only slightly increased in granulomatous inflammation. Infestation of the central nervous system and the heart can lead to death. In the USA and in Europe, about 3 % of all lung transplants are performed due to granulomatous inflammation in the lung. The indication for this is largely fibrosis of the lungs arising from sarcoidosis, pulmonary hypertension or cystic transformation with mycetomas. A not exactly small proportion of sudden cardiac deaths in young people are due to sarcoidosis. If the central nervous system is involved, insults are often the result. The development of a leukoencephalopathy is particularly feared, because this is usually fatal.
