What is Human T-Lymphotropic Virus 1?
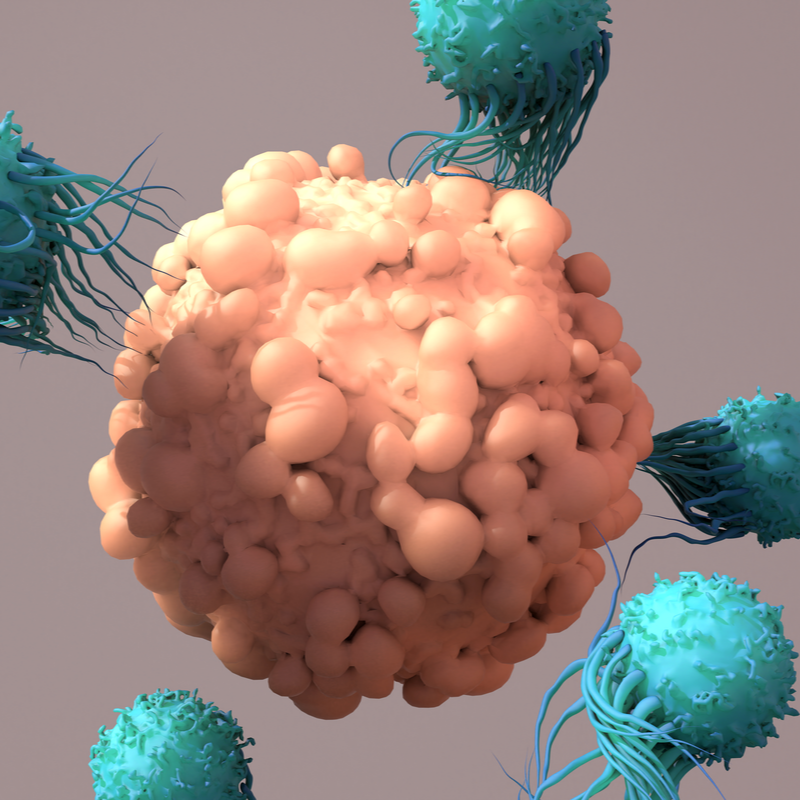
The human T-lymphotropic virus 1 is also abbreviated as HTVL-1. It is a retrovirus assigned to the oncoviruses. The virus mainly infects CD4-positive T lymphocytes. In many cases, infection with the virus triggers T-cell leukaemia. A manifestation of infection with the virus through an attack on the nervous system is also possible.
What is the morphology of human T-lymphotropic virus 1?
The virus is icosahedral and surrounded by a lipid envelope. It measures approx. 100 nm in diameter. The virus is constructed so that the envelope contains the matrix, has the capsid, the capsid antigen and a central core, with a single-stranded RNA.
How widespread is human T lymphotropic virus 1?
Estimated are about 15-20 million people worldwide infected with HTLV-1 . Compared to the infection figures for HIV, this is about 13 million fewer. HTLV-1 infection has so far largely been confined to certain endemic areas, whereas the HI virus has spread explosively into a pandemic mainly in the 1980s. This is mainly due to the fact that the transmission of HTLV-1 is much less efficient. Known risk areas for human T-lymphotropic virus 1 are:
- Japan, with the southern islands being particularly at risk,
- the Caribbean and Central America,
- certain regions of Equatorial Africa,
- certain regions of South America,
- certain populations in the USA.
In
the European countries, on the other hand, HTLV-1 is practically not found at all
, except for immigrants from the endemic areas mentioned above, who already carry the
virus when they enter the country.
How is the human T-lymphotropic virus 1 transmitted?
The following three main ways in which the virus can be transmitted are known:
- a postnatal infection of an infant through receiving breast milk from an infected mother.
- by passing on infected blood products via transfusions.
- through sexual contact, whereby transmission here usually occurs through the male.
What are the symptoms of human T-lymphotropic virus 1?
Human T-lymphotropic virus 1 can be the cause of the following two diseases:
- Adult T-cell leukaemia: This is a highly aggressive form of Non-Hodgkin lymphoma. The disease can progress from acute to chronic . The acute form usually leads to death within a few months. Typical symptoms are itchy, livid lesions of the skin and an infection of the entire internal organs as well as bones and nerves.
- Tropical spastic paraparesis: In this disease, which can be triggered by the virus , the focus is especially on neurological changes . These include urinary and faecal incontinence, paraparesis and back pain. Other symptoms may include uveitis, keratoconjunctivitis, psoriasis and arthritis.
How is human T-lymphotropic virus 1 diagnosed?
A diagnosis must be made with the help of laboratory tests of cerebrospinal fluid, EDTA blood, bone marrow, skin biopsy and/or lymph node tissue. The virus can be primarily detected with a PCR test. As an alternative the p19gag antigen test can be used.
A proven infection with the human T-lymphotropic virus 1 leads to a ban on blood donations and organ donations for affected persons. An education about practising unprotected sexual intercourse must be provided . An infected mother should not breastfeed, but bottle-feed her infant.
How is human T-lymphotropic virus 1 treated?
The treatment depends on the disease that has been triggered. In the first instance, a combination therapy is used. Here, reverse transcriptase inhibitors or also lamivudine with interferon alpha are used. This therapy is carried out for 6 to 12 months. In addition, it is possible to administer valproic acid to further reduce the viral load. If there is an acute adult T-cell leukaemia , an aggressive chemotherapy is usually tried as a treatment .
How can human T-lymphotropic virus 1 be prevented?
A vaccination against this virus does not yet exist. At the present time, no research is being conducted to bring a vaccine onto the market in the near future. Since is primarily transmitted through blood and unprotected sexual intercourse, the use of condoms is still the best and most effective measure to prevent the virus. Infected mothers should not breastfeed their babies. Drug users are also at risk of becoming infected with the human T-lymphotropic virus 1 if they share needles with others. Drug users should always use their own needles, also to prevent other infectious diseases.
What is the prognosis for diseases caused by human T-lymphotropic virus 1?
In an acute adult T-cell leukaemia, where the lesions of the skin are in the foreground, the prognosis is quite good. The mean survival rate is then more than 20 years. If the focus is on the leukaemic disease, the survival time is less than 1 year after the diagnosis is made.
In tropical spastic paraparesis, the prognosis is much better. However, secondary diseases such as arthritis, psoriasis and uveitis can reduce the patient's quality of life enormously. However, deaths are much less frequently associated with human T-lymphotropic virus 1.
Is there an obligation to report human T-lymphotropic virus 1?
According to the Infection Protection Act in Germany, there is no obligation to report human T-lymphotropic virus 1.
