What is liver carcinoma?
Liver carcinoma is also colloquially called liver cancer and refers to a malignant disease of the liver cells. In Germany, liver carcinoma is considered a relatively rare tumour disease, which on average affects men over 70 years of age and women over 72 years of age with above-average frequency. Doctors can also call a liver carcinoma a primary liver cancer because it originates in the liver. Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer. Doctors speak of secondary liver cancer when daughter tumours (so-called metastases) from other malignant tumours have settled in the liver. This can be the case, for example, with bowel cancer or stomach cancer. Primary and secondary liver carcinomas differ from each other in terms of their course and treatment.
What is the function of the liver?
The liver (hepar) is the heaviest human organ and is considered the largest gland in the human body. Lying in the right upper abdomen, it is located directly below the diaphragm and is protected by the lower ribs. As a central metabolic organ, the liver fulfils vital tasks, such as the production of bile, which is needed for the digestion of fats, or serves as the body's detoxification centre, where harmful substances such as drugs or alcohol are broken down.
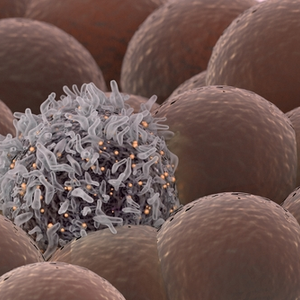
How does liver cancer develop?
In Germany, most cases of liver cancer (HCC) are due to a so-called shrunken liver (liver cirrhosis). Liver cirrhosis refers to a scarring remodelling of the liver tissue that can develop as a result of long-term liver damage and/or liver inflammation (hepatitis) and also leads to the destruction of liver cells. In less than 20 percent of all cases of liver cancer, there is no liver cirrhosis.
Liver cirrhosis and liver cancer occur mainly due to the following causes:
- chronic alcohol abuse: regular alcohol consumption can lead to chronic inflammation of the liver tissue (alcoholic hepatitis), which in turn can be the cause of liver cirrhosis and liver cancer.
- chronic viral infections, especially with hepatitis C or hepatitis B viruses: While hepatitis B viruses are transmitted through body fluids and cause inflammation of the liver (hepatitis), chronic hepatitis B infections occur predominantly in Asia and Africa, while chronic hepatitis C infections are common, especially in the USA, Europe and Japan.
- Occupational factors: Some occupational groups are at increased risk of cancer. These are mainly occupations that carry an increased risk of infection with hepatitis B and C, such as medical workers who come into increased contact with body fluids. Vaccinations, for example against hepatitis B infection, can reduce the risk.
- fatty liver disease, which is caused by severe overweight (obesity) and/or type 2 diabetes mellitus: The mould toxin aflatoxin, which can be contained in contaminated cereal products, for example, can also contribute to the development of liver carcinoma. However, aflatoxin is mainly found in tropical and subtropical countries with warm, humid climates. In addition to aflatoxin, obesity and diabetes mellitus can also clearly increase the risk of HCC.
- Medication: If sex hormones, such as oral contraceptives or anabolic steroids for muscle building are taken over a longer period of time, they can lead to liver damage and promote the growth of liver tumours.
- genetic factors: Various hereditary metabolic diseases can increase the risk of liver cancer. These include above all the so-called iron storage disease (haemochromatosis), in which the body is almost overloaded with iron due to increased iron absorption.
What symptoms can liver carcinoma cause?
In the early stages, liver cancer usually causes few symptoms, which is why liver cancer is usually discovered when the tumour has already reached a certain size. At this stage, the following rather unspecific complaints may occur.
- a feeling of pressure in the right upper abdomen,
- unwanted weight loss,
- a yellowing of the eyes as well as the skin,
- an increase in the circumference of the abdomen due to water retention (abdominal dropsy, ascites).
How is liver carcinoma diagnosed?
First of all, the attending physician will take a medical history by asking about previous illnesses, lifestyle habits and complaints. The doctor will also ask if the patient regularly takes medication. Then the abdominal cavity is palpated during a physical examination. In addition, laboratory tests can provide information about possible liver damage.
If these examinations confirm the suspicion of an existing liver carcinoma, further imaging procedures are carried out. A three-phase contrast-enhanced cross-sectional imaging procedure can be used, but a tissue sample (liver biopsy) can also be taken.
How can liver carcinoma be treated?
Depending on the size of the tumour, a liver carcinoma is usually removed completely by surgery. If the tumour has already spread considerably or if it is a case of end-stage liver cirrhosis, a liver transplant can also be considered. However, the patient usually has to wait a long time due to the lack of availability of a suitable donor organ.
Alternative treatment methods for liver carcinoma consist of so-called transarterial chemoembolisation (TACE). After the administration of a chemotherapeutic agent, the blood supply of the tumour cells is closed off by gel foam or small metal spirals. However, the tumour can be destroyed by heat using a so-called radiofrequency blation (RFA) or microwave ablation (MWA). However, this application method can only be performed on tumours with a maximum size of 5 cm.
