Mast cell activation symptoms are common in long-COVID patients
A new study in the International Journal of Infectious Diseases shows that mast cell activation symptoms are highly prevalent in Long COVID sufferers and are almost identical in nature and severity to mast cell activation syndrome (MCAS).
This finding may explain why many long-COVID patients report a variety of seemingly unrelated symptoms - from fatigue and brain fog to intestinal discomfort, skin reactions and palpitations.
What are mast cells and why do they play a role in COVID-19?
Mast cells - the "guardians" of the immune system
Mast cells are immune cells that are found in almost all tissues of the body. They release messenger substances such as histamine, tryptase or prostaglandins to react to pathogens or injuries.
This reaction is normally short-lived and protective - it triggers inflammatory signals that activate the immune system.
When protective mechanisms get out of control
In mast cell activation syndrome (MCAS), however, there is a permanent or excessive release of these messenger substances.
This leads to symptoms such as:
-
Reddening of the skin, hives, itching
-
Gastrointestinal complaints
-
Palpitations, dizziness
-
Tiredness, brain fog
-
Breathing difficulties
Exactly these symptoms are also found in Long COVID patients.
The study: Mast cell activation in long-COVID
Objectives and study design
The team led by Leonard B. Weinstock investigated whether long-COVID symptoms could be due to mast cell activation.
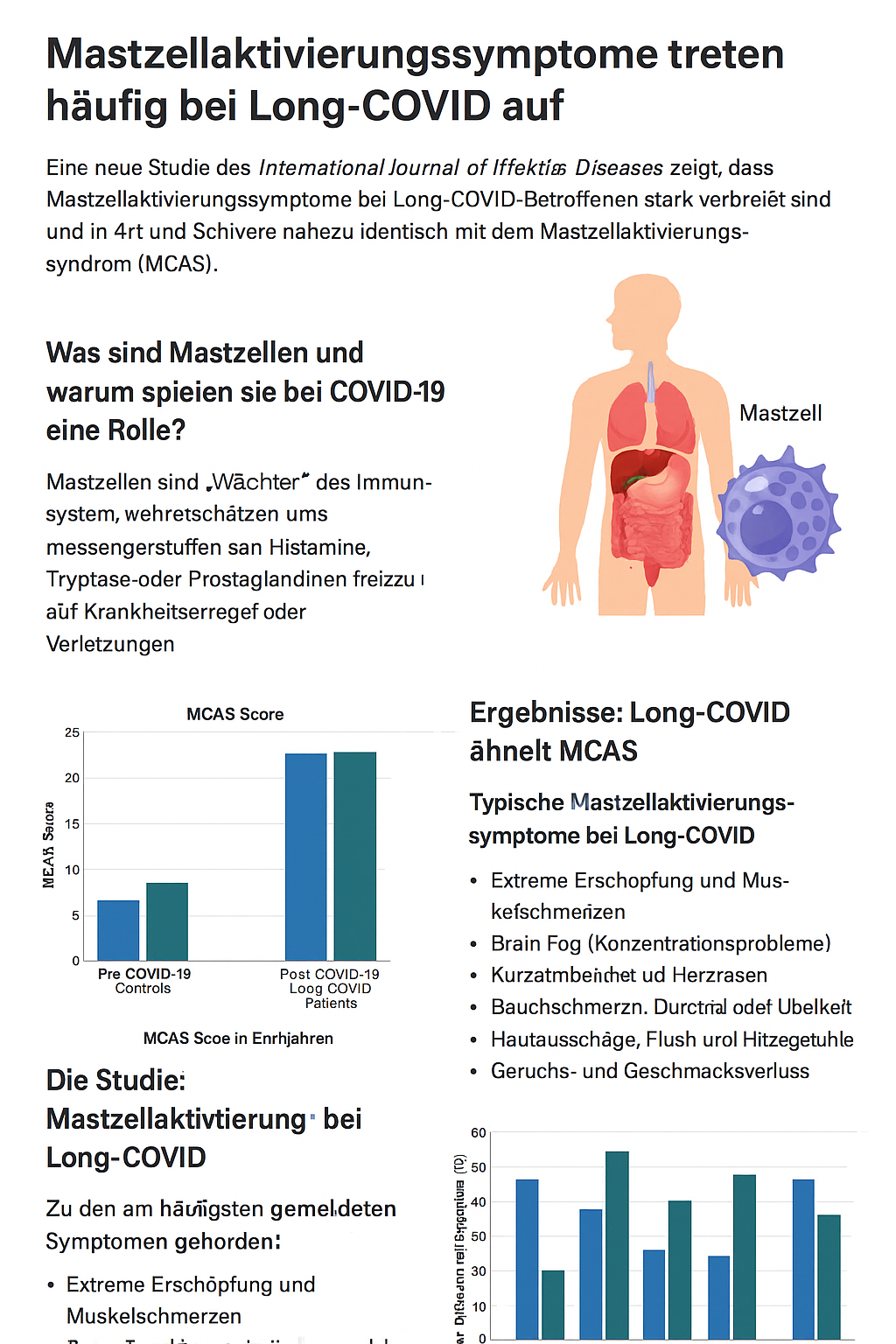
To this end, 136 long-COVID patients, 136 healthy controls and 80 diagnosed MCAS patients were surveyed.
The participants completed online questionnaires on symptoms, severity, fatigue and quality of life, both before and after the COVID-19 infection.
Participant groups and methods
The researchers compared the data in three steps:
-
Long-COVID symptoms before infection with healthy controls.
-
Long-COVID symptoms after infection.
-
These results with the symptoms of untreated MCAS patients.
Over 50 different symptoms were recorded, categorised by organ system (e.g. skin, lungs, nervous system).
Results: Long-COVID is similar to MCAS
Comparison of symptoms: Long-COVID vs. MCAS
Before the infection, the Long-COVID participants did not differ significantly from the control group.
After the infection, however, there was an increase in:
-
Number of symptoms,
-
Severity,
-
and the number of affected organ systems** increased significantly**.
The overall values of the Long COVID group were almost identical to those of the untreated MCAS patients (see Table 3, page 4 of the study).
Typical mast cell activation symptoms in Long-COVID
The most frequently reported symptoms included:
-
Extreme fatigue and muscle pain
-
Brain fog (concentration problems)
-
Shortness of breath and palpitations
-
Abdominal pain, diarrhoea or nausea
-
Skin rashes, flushing and feelings of heat
-
Loss of smell and taste
As shown in Figure 4 (page 8), almost all symptoms showed a significant increase after COVID-19.
Quality of life and fatigue levels
While healthy control subjects and Long COVID participants reported similar quality of life scores (~75/100) before the infection, these dropped to 40 points after COVID-19.
The fatigue score also almost doubled from 16.6 to 34.5 points.
What does this mean for those affected?
Parallels to mast cell activation explain many long-COVID symptoms
The researchers suspect that SARS-CoV-2 triggers excessive mast cell activation.
This leads to a chronic inflammatory reaction that could explain many long-COVID symptoms - from neurological symptoms to digestive problems.
Possible mechanisms:
-
Cytokine storm as a trigger for genetic changes in mast cells
-
Activation by viral components or autoantibodies
-
Dysregulated signalling pathways that keep mast cells permanently active
Possible treatment approaches
The authors suggest testing therapies that are already used in MCAS:
-
Antihistamines (H1/H2 blockers)
-
Mast cell stabilisers such as cromoglicic acid
-
Flavonoids (e.g. quercetin, luteolin)
-
Vitamin C and D
-
Low-dose naltrexone (LDN) to inhibit inflammation
Some small studies have already shown positive effects of these treatments in long-COVID patients.
Limitations of the study and outlook
The study is based on self-reporting and online surveys, which may cause certain biases.
In addition, almost 90 % of the participants were female, which could limit transferability.
Nevertheless, the results provide important evidence that mast cell activation may play a central role in long-COVID pathophysiology.
Further clinical studies with objective measurements of mast cell mediators and controlled treatment trials are urgently needed.
Frequently Asked Questions (FAQ)
1️⃣ What is mast cell activation?
An excessive or uncontrolled release of inflammatory mediators from mast cells that can cause numerous symptoms throughout the body.
2️⃣ What symptoms are typical of mast cell activation in long-COVID?
Fatigue, brain fog, skin reactions, gastrointestinal complaints, dizziness, palpitations, breathing problems and loss of smell.
3️⃣ Is Long-COVID the same as MCAS?
No. Long-COVID shows similar patterns but does not automatically fulfil the diagnostic criteria for MCAS.
4️⃣ Can medication for MCAS help with long-COVID?
Initial reports suggest that antihistamines and mast cell stabilisers may be helpful.
5️⃣ Why does Long COVID affect women more often?
Women's immune systems tend to react more strongly, which may play a role in autoimmune and allergy-like diseases.
Conclusion
The study by Weinstock et al. clearly shows:
👉 Mast cell activation symptoms occur frequently in long-COVID - and are very similar to mast cell activation syndrome (MCAS).
This suggests that long-COVID may not only be a late viral consequence, but also a chronic inflammatory disorder of the immune system.
Targeted therapies against mast cell overactivity could therefore represent an important therapeutic approach.
🔗 So urce: Weinstock L.B. et al, International Journal of Infectious Diseases, 2021
