What is penile cancer?
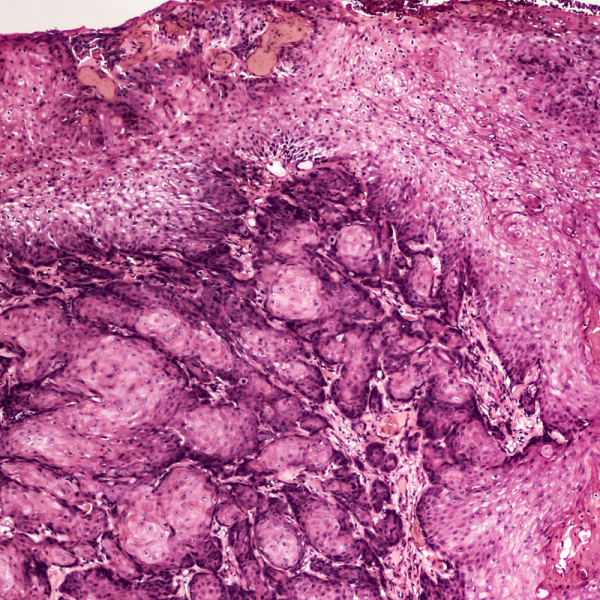
Penile cancer is also medically called penile carcinoma. In almost 95 percent of all cases, it is a squamous cell carcinoma, i.e. a malignant tumour. In contrast to other cancers, penile cancer occurs rather rarely and only affects about a few hundred men in Germany every year, mostly from the age of 60. Penile cancer is even rarer in men under 40.
Penile cancer can make itself felt through bleeding, skin changes, lumps, hardening or swelling of the penis. If diagnosed early, penile cancer can be operated on and has a good prognosis for cure, provided that all malignant tumour cells have been removed. If, on the other hand, penile cancer is diagnosed at a stage where the tumour has already metastasised, palliative chemotherapy must be administered and the prognosis worsens according to the stage of the tumour.
How does penile cancer develop?
In most cases, penile cancer belongs to squamous cell carcinoma. This malignant cancer is caused by the degeneration of the cells of the outermost layer of the skin. Penile cancer forms particularly frequently on the foreskin and the glans. If the tumour remains untreated, it can even spread to the corpus cavernosum, the prostate and/or the urethra. The tumour cells can migrate to the inguinal lymph nodes and the pelvis via the lymphatic system. At a later stage, the tumour can also metastasise via the blood to other organs such as the lungs or the skeleton.
Into which tumour stages is penile cancer classified?
Penile cancer is classified according to the international TNM classification (T=tumour, N=lymph node involvement, M=metastases). This describes the respective cancer stage on the basis of internationally recognised standards. In addition to the question of how deep the tumour has already penetrated into the cell tissue (infiltration), it is also a question of whether the lymph nodes are affected and whether metastases have formed in other organs:
- T1: The tumour is superficial and only limited to the connective tissue.
- T2: The tumour has affected the corpora cavernosa.
- T3: The tumour has affected the urethra.
- T4: The tumour has affected neighbouring structures, such as the prostate.
- N0: The lymph nodes are still tumour-free.
- N1: The tumour has only affected one lymph node so far and is still regionally limited.
- N2: The tumour has spread to several inguinal lymph nodes.
- N3: The tumour has spread to the pelvic lymph nodes or is growing beyond an already affected lymph node.
- M0: The tumour has not yet metastasised.
- M1: The tumour has already metastasised to other organs.
What risk factors favour the development of penile cancer?
Doctors have not yet been able to adequately clarify the causes of penile cancer. However, they assume that the following factors can favour the development of penile cancer:
- advanced age,
- Smoking,
- poor hygiene: especially pre-skin sebum (smegma) can contribute to the development of penile cancer,
- human papilloma virus (HPV) and genital warts, which can be caused by HPV,
- Foreskin stenosis (phimosis), which causes some foreskin sebum to always remain between the glans and the foreskin and can lead to chronic infection of the glans,
- Mucosal changes such as leukoplakia, which is a whitish change in the mucous membrane, can be the beginning of penile cancer.
Men over the age of 45 can have an annual screening examination for prostate cancer. Not only is the prostate examined, but also the external genital organs. If the disease is suspected, further imaging procedures will be ordered.
What are the symptoms of penile cancer?
Because it usually grows slowly, penile cancer does not cause pain or other symptoms, especially at the beginning of the disease. The following symptoms can indicate penile cancer:
- a swollen or hardened foreskin or glans,
- small ulcers or nodules on the glans,
- Skin that bleeds easily and does not want to heal
If these symptoms increase in intensity, it may mean that the tumour is already in an advanced stage. If the tumour has already affected the lymph nodes, this can usually be felt in the groin region.
How is penile cancer diagnosed?
The treating urologist will first take the patient's medical history. This is usually followed by a thorough examination of the penis, including palpation of the lymph nodes in the groin. If penile cancer is suspected, a tissue sample is taken for microscopic examination in the laboratory (biopsy). If the biopsy shows that penile cancer is present, further examinations are carried out to find out to what extent the cancer has already spread to other organs. Imaging tests such as ultrasound (sonography), magnetic resonance imaging (MRI) or computer tomography (CT) are used. An X-ray is taken if there is a suspicion of cancer in the lungs. If bone metastases are suspected, the doctor will do a skeletal scintigram.
How is penile cancer treated?
Penile cancer is usually only treated in specialised centres because it is a rather rare type of cancer. The urologist will try to remove the tumour tissue completely by surgery. If the tumour is still in an early stage, surgery can also preserve the penis and its function. If it is a small carcinoma, this can also be destroyed with a laser. If, on the other hand, it is a penile carcinoma that has already penetrated into deeper layers or has already metastasised to other organs, a partial or complete penile amputation may be necessary to cure the patient.
At a very advanced stage, when it is no longer possible to save the patient, radiation or chemotherapy is usually used. This is intended to alleviate the patient's discomfort and pain (palliative therapy).
